A Novel and Integrative Nutritional Approach to Neurologic Disorders and Autoimmunity
Protomorphology.jpg
Integrative Veterinary Care Journal, Volume 7, Issue 2, Spring 2017
Last year, funding for four grants was approved by the AKC Canine Health Foundation as part of an Epilepsy Research Initiative. This initiative is designed “to provide the veterinary community and dog owners with improved methods for preventing and treating epilepsy in dogs.”1 One of the grants will look at the effects of nutrition (ketogenic diet) on the reduction of seizure frequency and/or the severity of seizures in drug-resistant dogs.2 It is exciting that research is starting to focus on nutritional solutions to optimize the health of our pet patients.
Functional nutrition through the use of tissue-specific protein extracts (ProtomorphogensTM) should also be explored as an integrative nutritional approach to neurologic challenges. Cells need food to function. To function optimally, nerve cells need to be exposed to the right quality and quantity of a variety of nutrients. These nutrients should ideally come from the food an animal eats. Every part of the animal is important to the health and wellness of the predator: “A victim to a carnivore's table is frequently eaten entirely.”3 Organ and glandular tissue is especially essential; it has more DNA per gram than skeletal muscle, and it contains protein, vitamin and mineral profiles unique to that organ.4 When an animal consumes the brain and nervous tissue of its prey, that meal will uniquely nourish the brain and nervous tissue of the predator.
Protomorphogens
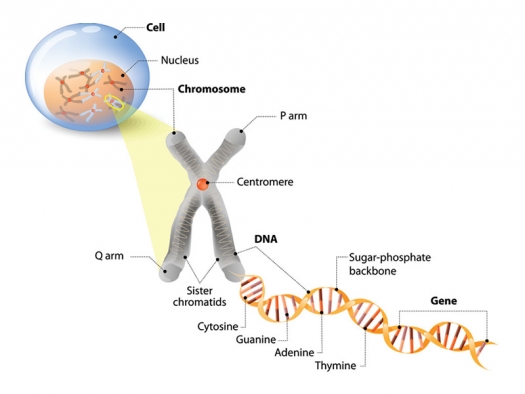
Organotherapy, the treatment of disease with organs and glands, was studied by human endocrinologists in the early part of the 20th century. Dr. Royal Lee, DDS, an early pioneer in human nutrition, proposed that glands and organ tissue could be effective beyond their unique vitamin and mineral content. He believed that animal extracts supported cellular health at the level of the nucleus, and in an unbalanced system these extracts could activate cells to repair. In 1947, six years before Watson and Crick defined DNA and the double helix, Dr. Lee proposed his theory of Protomorphology.5
Dr. Lee described Protomorphogens as “cell determinants” from organ or glandular tissue (“proto” = primary or original; “morphogen” = that which organizes form). He believed them to be the smallest functional units of the chromosome – cell-specific nucleoproteins that provided the blueprint and framework upon which a cell was constructed: “Suppose you have a building that is deteriorating. The manager will call in the repair crew. If the crew doesn’t have a blueprint, the repair won’t be adequate.” According to Dr. Lee, Protomorphogens (PMGs) served the cell like the seeds of a plant by helping with normal tissue function and catalyzing cell repair.4,6
Autoimmunity and PMGs
In Dr. Lee’s opinion, it wasn’t that there were so many autoimmune conditions; it was that so many chronic health challenges reached the autoimmune phase. Autoimmunity is inevitable in chronic disease as tissues became necrotic and decayed. Autoimmunity is the result of a failure to heal. Dr. Lee theorized that when tissue was damaged – as is in the case of a coronary occlusion – nucleoproteins from the necrotic tissue would leak into the bloodstream. Antibodies would respond to these “foreign” antigens and the patient would essentially become “allergic” to his own heart. The patient’s bloodstream would begin to carry antibodies to the heart, impairing the repair of the heart itself.6 This is autoimmunity. Dr. Lee envisioned the autoimmune cascade as the body’s attempt to preserve itself, even though its effects could be more deadly than the disease itself.
Dr. Lee saw the solution to autoimmunity in the nucleoproteins of the cell. He hypothesized that a heart specific protein (Cardiotrophin PMG®) could be given orally to lower circulating antibodies to the heart tissue. Once in the gastrointestinal tract, the PMG would act as a decoy to the immune system, drawing cardiac auto-antibodies away from the heart, thus relieving the autoimmune attack on the heart, and giving the heart the opportunity to heal as therapeutic nutritional support is introduced.6
The theory of Oral Tolerance
Dr. Lee’s theory is strikingly similar to research that is being conducted today in the field of Oral Tolerance. Defined in 1977,7 Oral Tolerance is a state of non-responsiveness to an antigen.8 According to Oral Tolerance, when an antigenic protein is ingested orally, it is taken up by the Peyer’s patches in the ileum and presented to the bloodstream via dendritic cells. The body’s natural immune response is then used to induce regulatory cells directed at that antigen.9 Oral Tolerance works by one of three mechanisms:
- activating regulatory cells, which suppresses symptoms;
- rebooting the immune system so it doesn’t react to the antigen (anergy); and
- deleting reaction to the antigen altogether (clonal deletion).
Results are dose dependent. Higher doses lead to anergy or deletion, and low doses support suppression of symptoms.8 Continuous administration enhances the effect significantly by upregulating IL-10 and TGF-β.10
Oral Tolerance has been used in animal models to block the development of disease. It has been found to have beneficial effects in animal models of arthritis, colitis, diabetes, uveitis, myasthenia gravis, thyroiditis and EAN (Experimental Allergic Neuritis).
In inflammatory conditions that have not yet reached the autoimmune phase, Oral Tolerance can protect the body against the self-antigen produced in response to inflammation.10
Neurologic implications
Nervous system trauma induces auto-antibody production as part of the natural healing process. Research has shown that anti-brain antibodies are produced following traumatic brain injury and spinal cord trauma. They have been found to be big players in neurologic disorders like SLE and MS.11 Patients with CNS paraneoplastic syndromes, kids with autism, and people exposed to environmental toxins have been found to have these antibodies in their serum. Some antibodies can be traced back to tissue injury occurring years before the onset of disease. Brain autoantibodies are also a produced as part of the natural aging process.11,12
Oral Tolerance can be used to treat some forms of neuroinflammation. Tissue-specific antigens like oral MBP (myelin basic protein) given orally to rats with induced strokes were shown to decrease stroke size, most likely because of the downregulation of inflammation. Both small and large doses of MBP have been shown respectively to suppress EAE (Experimental Allergic Encephalomyelitis) and be protective, non-detrimental and beneficial in EAE animal models. Findings from these studies indicate that:
- the effect of Oral Tolerance is dose-dependent;
- purified proteins are most effective;
- the more frequently and consistently an oral antigen is given, the more effective it is;
- early therapy yields better results; and
- combination therapy with medications may provide better results.11
Oral Tolerance and Protomorphogens
Protomorphogens are cell-specific proteins. One of the ways they may work in the body is through Oral Tolerance. Unlike Oral Tolerance, Protomorphology was outcome-based. Patients who took PMGs experienced symptom relief. Dr. Lee did not have today’s science to prove his theory, but he was able to trace heart sounds before and after the administration of a heart PMG. He found the sounds amplified shortly after oral administration of the PMG, which he theorized was due to increased pressure and better cardiac contractility. As with a heart PMG, patients with chronic coughs or TB could take a lung PMG; patients with digestive issues could take a pituitary PMG; and patients with nervous disorders could take a nervous system PMG to support healing.
Putting Protomorphogens into practice
It is not difficult to integrate PMGs into a patient care plan. They come in tablet form, are palatable, and for most animals (even cats) they can be given as treats. Animals with seizure disorders, neuritis, degenerative myelopathy, nerve trauma, head injury and other nervous system-related injuries or conditions are excellent candidates for this type of targeted nutritional therapy. In our experience, and in the experience of other practitioners, PMGs have supported animals dealing with any type of acute tissue injury, toxin exposure, or chronic condition. Many patients see symptomatic improvement when a PMG is added to their nutritional plan.
The following is a guideline for PMG use in veterinary patients:
- PMGs should be given on an empty stomach if possible. It’s important for the PMG to reach the Peyers patches in the ileum in order for the immune system to recognize it.
- PMGs can be given in twice daily or single daily doses. Oral tolerance suggests a higher single dose will help not only with symptoms, but may affect anergy or clonal deletion.
- The general dosage is as follows, but should be tailored to the individual:
- Large (>50#) 4/day
- Medium (20-50#) 3/day
- Small dog or cat (<20#) 2/day
- Start the PMG at half the recommended dose for the first seven to ten days, then increase to full dose (as tolerated). Histamine response (itch, digestive upset) is uncommon but can happen. If histamine response occurs, antihistamines or a beef liver fat extract (VF Antronex®) can help detoxify histamine from the liver; the PMG may be continued at a reduced dose.
- Duration of treatment depends on the individual. In the case of chronic conditions, PMGs may be given long term (years). In acute situations, the treatment course may be shorter (several months to a year).
While PMGs contain minerals, nucleotides (the components of nucleic acids like RNA and DNA), and peptides (short chains of amino acids), they don’t provide the complex nutritional tools the body needs for full function.4 Their job is to help maintain normal cell metabolism and cell cycling, and to potentially enable tissue-specific immune downregulation. It’s important that other whole functional foods are provided along with a PMG to promote full healing and repair to damaged tissues.
Conclusion
Protomorphogens are proprietary glandular extracts (Standard Process) that offer a novel and safe approach to supporting nervous system health. As a form of Oral Tolerance therapy, they lack toxicity, are easy to administer, and are antigenspecific; current medical therapies for people and animals with autoimmune and inflammatory conditions often depend on non-specific immune-suppression with medications – some of which can have undesirable effects.10 In practice, Protomorphogens can profoundly support patients with nerve-related and other conditions by encouraging healing over time, especially if they are used as an integrative approach to overall patient care.
- JAVMA, Sept 1 2014, Vol 245, Number 5:478.
- ”Canine Health Foundation Awards Six New Grants to Study Epilepsy and Reproductive Diseases in Dogs.” AKC 5/9/2016.
- Patton, Richard. Ruined by Excess, Perfected by Lack: The paradox of pet nutrition. Nottingham University Press, 2011.
- ”Protomorphogen™ Extracts Fact Sheet.”
- Royal Lee and William A. Hanson. Protomorphology: The Principles of Cell Auto-Regulation. Lee Foundation for Nutritional Research, Milwaukee WI 1947.
- ”Dr. Royal Lee on Protomorphogens”. Digital re-recording from source tapes recorded in September 1957. Applied Nutritional Services.
- Vaz NM, Maia LC, Hanson DG, Lynch JM. 1977. “Inhibition of homocytotrophic antibody responses in adult inbred mice by previous feeding of the specific antigen”. J. Allergy Clin Immunol, 1977, 60(2):110-115.
- ”Food for Thought: Can Immunological Tolerance Be Induced to Treat Asthma?” Lauren Cohn Department of Internal Medicine, Section of Pulmonary and Critical Care, Yale University School of Medicine, New Haven, CT Am. J. Respir. Cell Mol. Biol. Vol. 24, pp. 509–512, 2001.
- ”Antigen-Specific Strategies for Auto-Immune Disease Treatment: Oral Tolerance, ImmuneWorks”, uploaded February 2012.
- Ana M, C. Faria1 and Howard L. Weiner2. “Oral tolerance: Therapeutic implications for autoimmune diseases”. Departamento de Bioquı´mica e Imunologia, Instituto de Cieˆncias Biolo´gicas, Universidade Federal de Minas Gerais, Av. 1Departamento de Bioquı´mica e Imunologia, Instituto de Cieˆncias Biolo´gicas, Universidade Federal de Minas Gerais, Av.Antonio Carlos, 6627, Belo Horizonte,MG 31270-901, Brazil, and 2Harvard Medical School, Center for Neurologic Diseases, Brigham and Women’s Hospital, 77 Avenue Louis Pasteur, Boston, MA 02115, USA ISSN 1740-2522 print/ISSN 1740-2530 online q 2006 Taylor & Francis.
- Kobeissy FH. “Autoantibodies in CNS Trauma and Neuropsychiatric Disorders: A New Generation of Biomarkers.” Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects. Ch. 29 editor. Boca Raton (FL): CRC Press/Taylor & Francis; 2015.
- Elamin NE1, Al-Ayadhi LY. “Brain autoantibodies in autism spectrum disorder.” Biomark Med., 2014; 8(3):345-52. doi: 10.2217/bmm.14.1.
Originally published in Integrative Veterinary Care Journal, Volume 7, Issue 2, Spring 2017. Used with permission.



