By late 2018, it was estimated that 17 million people have had their DNA analyzed by companies like 23andMe and Ancestry. And that number is expected to grow by at least a million every month. You might even know someone who has done one. And you might be wondering: What’s the point?
The truth is, big questions need big data. DNA repositories are now getting so big that the information gained from them can be used in ways we thought we’d only see in science fiction movies just decades ago. And one of the most undeniably significant applications of this data is precision medicine.
Humans are incredibly complex beings — but until recently, modern medicine has treated every patient as if they were one and the same. Doctors had no idea who would benefit from certain drugs, who was at risk of developing Alzheimer’s disease, or even seemingly trivial things like who would go bald. While we certainly have a long way to go in terms of personalizing medicine for each and every patient, recent research suggests that therapeutic peptides could pave the way.
Peptide therapy has been gaining great interest and popularity in recent years as a novel approach to slow down aging and treat diseases. In this article, we’ll discuss what peptide therapy is and how it might benefit your health.
What are peptides?
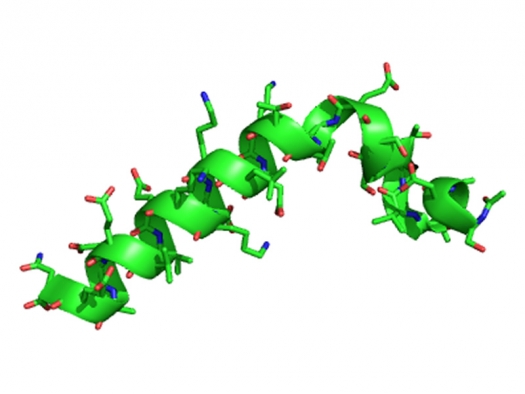
Peptides can be thought of as small proteins (less than 50 amino acids long) that typically act as highly specific signaling molecules in many crucial functions in our bodies, including hormone production, cell signaling, and cell-to-cell communication.
Peptides often have attractive properties and pharmacological profiles that make them highly desirable as starting points for drug design and development. There are several advantages of using these small receptor-binding molecules as therapeutics, a few of which are:
- Low toxicity
- High chemical and biological diversity
- High potency and specificity
- Good efficacy, safety, and tolerability
- Broad range of targets
- Low accumulation in tissues
But perhaps the biggest advantage of therapeutic peptides is the fact that they are amenable to rational design. Therapeutic peptides can be designed to be involved in virtually any cellular process. This means that they can be designed to block interactions of proteins as long as enough of the sequence of the target site is known and conditions allow for the peptide to bind it.
Owing to these advantages as well the rapid developments in proteomics and bioinformatics, more than 7,000 naturally-occurring peptides have been identified, and the global peptide therapeutics market is expected to reach over $50 billion by 2024.
But why has it taken so long for peptides to be as well known as they are today? The idea of using peptides for drug design was largely ignored by pharmaceutical companies due to several intrinsic weaknesses, such as:
- Poor chemical and physical stability
- Small size, which makes them vulnerable to degradation
- Prone to hydrolysis and oxidation
- Tendency for aggregation
- Short half-life, fast elimination
- Low oral bioavailability
- Low membrane permeability
- Higher production costs
Because of these weaknesses, naturally-occurring peptides are not directly suitable for use as therapeutics. However, thanks to recent advances in technology, numerous improvements have been made to the stability, transport, oral availability, and affinity profiles of peptides. These changes have renewed interest in peptides as potential therapeutic drugs.
What conditions can peptides therapy treat?
Peptides can be used to treat a wide range of illnesses. The list of potential conditions that can benefit from peptides is nearly endless, but here are just a few:
- Insomnia
- Inflammation
- Cancer
- Lyme disease
- Dementia
- Mold-related illness
- Joint injury
- HIV and chronic infections (HBV, HCV, CMV, etc.)
- Inflammatory bowel disease
- TBI
- Neurodegenerative conditions (Parkinson’s, MS, etc.)
- Erectile dysfunction, low libido
- Fibromyalgia
- Hashimoto’s thyroiditis
What types of peptide therapy are available?
Thymosins
The thymus gland is located behind your breastbone and between your lungs. Although it’s only active until puberty, it nevertheless plays a crucial role in the development of the immune system and in protecting the body against autoimmunity, a state in which the body’s immune system turns on itself. It is responsible for producing and secreting a hormone called thymosin, which stimulates the development of white blood cells called T-lymphocytes or T cells. For their roles in regulating the immune system, thymosins (also known as thymic peptides) are referred to as immune-modulatory peptides.
There are two thymic peptides commonly used in peptide therapy: Thymosin alpha 1 (Tɑ1) and thymosin beta 4 (Tβ4). Both of these peptides have been shown to have important clinical applications, such as in modulating immune responses, neuroplasticity, blood vessel formation, etc.
Let’s take a closer look at Tɑ1 and Tβ4.
Thymosin Alpha 1 (Tɑ1)
Thymosin alpha 1 is a naturally-produced peptide of 28 amino acids that can enhance the body’s ability to recognize and respond to foreign invaders. At the cellular level, Tɑ1 interacts with proteins called Toll-Like Receptors (TLRs), and it is the interaction with TLRs on dendritic cells and precursor T cells that results in immune-stimulating effects, including:
- Increased natural killer cell activity
- Increased expression of TH1-type cytokines
- Increased levels of cytotoxic T cells
- Reduced apoptosis of immune cells
- A shift of T helper cells to Type 1 T helper (TH1) cells
- Activation of dendritic cells
Studies show that immune dysregulation and/or immunosenescence (gradual deterioration of the immune system associated with age) results in an imbalance of TH1 and TH2. TH1 and TH2 cells secrete proteins called cytokines that exhibit protective effects. TH1 cells produce interferon (IFN) -g and interleukin (IL)-2 which tend to be pro-inflammatory, while TH2 cells produce IL-4, IL-5, Il-6, IL-10, and IL-13 which are anti-inflammatory.
TH1 and TH2 cells produce also differ in the types of immune responses they produce. TH1 cells typically deal with pathogens that get inside cells, such as bacteria and viruses. On the other hand, TH2 cells parasites that attack from outside the cells as well as toxins and allergens.
Both sides need to work together to have a well-balanced immune system. Neither should be in a dominant position. However, in some people, there is a prolonged period of time in which either TH1 or TH2 dominance occurs, leading to health problems. In particular, an increase in TH2 relative to TH1 has been linked to:
- Depression
- Insulin resistance, obesity, and diabetes
- Chronic fatigue syndrome / fibromyalgia
- Autoimmune disease
- Chronic infections (including Lyme, viruses, parasites)
- Oxidative stress
- Alterations in gut microbiota (i.e., dysbiosis)
- Food allergies
- Changes in sex hormone levels
- Zinc and other mineral deficiencies
- Cancer
This is one of the most significant clinical applications of Tɑ1. As an immunomodulator, Tɑ1 restores balance to the body by increasing TH1 and decreasing TH2, thus breaking the cycle of immune dysfunction so often found in these illnesses.
Several clinical studies have shown that Tɑ1 can benefit a broad range of conditions, some of which include:
- Boosting influenza antibody response
- Hepatitis B
- Sepsis
- Chronic obstructive pulmonary disease
- Melanoma
- Lung cancer
- Fungal infections
- Cystic fibrosis
- HIV-1
Due to the success of these clinical trials, drugs containing Tɑ1 have been approved for clinical use in over 35 countries (including the U.S.) and have had very few reports of adverse effects so far.
Thymosin Beta 4 (Tβ4)
Thymosin beta 4 is also produced in the thymus gland and is also the predominant form of thymosin in the human body. This means it can be found in all human cells, although it is typically found in high concentrations in wound tissue and in certain blood cells involved in wound healing.
Despite being a peptide of only 43 amino acids, Tβ4 is involved in modulating a wide range of regenerative activities. When the wound healing process begins, Tβ4 aids in:
- Promoting formation of new blood vessels to the injured area which carry essential reparative substances
- Increasing “good” inflammation that can help the wound heal faster
- Increasing the amount of cell-building proteins such as actin
- Restoring tissue structure and metabolism
- Promoting hair growth
- Reducing acute/chronic pain
From its anti-inflammatory properties, it’s easy to see why Tβ4 has such a huge potential in terms of clinical applications. So far, it has shown to be effective in several injury models, such as traumatic brain injury, stroke, spinal cord injury, a model of multiple sclerosis, diabetes, and cardiac damage resulting from reduced blood flow.
BPC 157
Pentadecapeptide BPC 157 is a synthetic, partial sequence of body protection compound (BPC), a protein that is naturally produced in the gastrointestinal (GI) tract. But the effects of BPC 157 extend beyond the GI tract – studies have also revealed that it has influences on:
- Tissue repair
- Formation of new blood vessels
- Maintenance of gut mucosal integrity
- Decreasing inflammatory mediators
- Growth rates
- Improving digestive function
- Traumatic brain injury
- Protecting the liver from toxins
The mechanism of BPC 157 is not yet fully understood. Some studies suggest that the peptide may be involved in the activation and regulation of vascular endothelial growth factor receptor 2 (VEGFR2), enhancement of the growth hormone receptor expression, and the FAK-paxillin pathway.
Like the other peptides we’ve discussed, BPC 157 has great potential for use in many chronic diseases like HIV, diabetes, cardiovascular disease, and autoimmune diseases. However, a majority of studies investigating BPC 157 have been done only in animal models, which do not always accurately predict effects in humans.
Cerebrolysin
Cerebrolysin is a nootropic, a synthetic drug that may enhance cognitive functions, such as memory, creativity, and motivation. Rather than being a single peptide, Cerebrolysin is a mixture of very small peptides derived from brains of pigs. The small size of Cerebrolysin means it can cross the blood-brain and the blood-cerebrospinal fluid barriers and directly act on the central and peripheral neurons.
The clinical value of Cerebrolysin comes from its neuroprotective effects. It has been shown to be effective when used for:
- Dementia including Alzheimer’s disease, mild cognitive impairment
- Recovery after a stroke
- Traumatic brain injury, concussion
- Spinal cord injury
- ADHD
- Treatment-resistant depression
Studies have indicated that Cerebrolysin is safe in humans for short-term use (up to 3 years). However, it has not been approved by the U.S. Food and Drug Administration (FDA).
What does the future look like for peptide therapy?
As we make advancements toward precision medicine, peptide therapy provides an innovative way to deliver highly potent and cost-effective medicine. Researchers continue to expand the number of peptide-addressable targets for which there are no drugs available, which simply indicate the nearly endless opportunities for new peptide therapeutics.
References
Recio C, Maione F, Iqbal AJ, Mascolo N, De Feo V. The Potential Therapeutic Application of Peptides and Peptidomimetics in Cardiovascular Disease. Front Pharmacol. 2017;7:526. Published 2017 Jan 6. doi:10.3389/fphar.2016.00526.
Global Peptide Therapeutics Market, Dosage, Price & Clinical Trials Insight 2024.
Komori, Teruhisa. The significance of proinflammatory cytokines and Th1/ Th2 balance in depression and action of antidepressants. Neuropsychiatry (2017) Volume 7, Issue 1.
Sami T. Azar, Hala Tamim, Hayfa N. Beyhum, M. Zouhair Habbal, Wassim Y. Almawi. Type I (Insulin-Dependent) Diabetes Is a Th1- and Th2-Mediated Autoimmune Disease. Clinical and Diagnostic Laboratory Immunology May 1999, 6 (3) 306-310.
Torres-Harding S, Sorenson M, Jason LA, Maher K, Fletcher MA. Evidence for T-helper 2 shift and association with illness parameters in chronic fatigue syndrome (CFS). Bull IACFS ME. 2008;16(3):19–33.
M. Ernberg, N. Christidis, B. Ghafouri, et al. Plasma Cytokine Levels in Fibromyalgia and Their Response to 15 Weeks of Progressive Resistance Exercise or Relaxation Therapy. Mediators of Inflammation, vol. 2018, Article ID 3985154, 14 pages, 2018.
Ishida H1, Ota H, Yanagida H, Dobashi H. An imbalance between Th1 and Th2-like cytokines in patients with autoimmune diseases--differential diagnosis between Th1 dominant autoimmune diseases and Th2 dominant autoimmune diseases. Nihon Rinsho. 1997 Jun;55(6):1438-43.
Miranda R. King, Anisa S. Ismail, Laurie S. Davis, David R. Karp. Oxidative Stress Promotes Polarization of Human T Cell Differentiation Toward a T Helper 2 Phenotype. The Journal of Immunology March 1, 2006, 176 (5) 2765-2772.
Chun Li1, Ji-Ying Chen, An-Lian Zhou. Correlation of serum sex hormone levels with Th1/Th2 balance as well as peripheral CD28, CTLA-4, PD-1 and PD-L1 expression in perimenopausal women. Journal of Hainan Medical University 2017; 23(10): 84-87.
Mbugi EV, Meijerink M, Veenemans J, et al. Effect of nutrient deficiencies on in vitro Th1 and Th2 cytokine response of peripheral blood mononuclear cells to Plasmodium falciparum infection. Malar J. 2010;9:162. Published 2010 Jun 14.
Lee N, Kim WU. Microbiota in T-cell homeostasis and inflammatory diseases. Exp Mol Med. 2017;49(5):e340. Published 2017 May 26.
Hae Lim Lee, Jeong Won Jang, Sung Won Lee, Sun Hong Yoo, Jung Hyun Kwon, Soon Woo Nam, Si Hyun Bae, Jong Young Choi, Nam Ik Han & Seung Kew Yoon. Inflammatory cytokines and change of Th1/Th2 balance as prognostic indicators for hepatocellular carcinoma in patients treated with transarterial chemoembolization. Scientific Reportsvolume 9, Article number: 3260 (2019).
Perkel, Jeffrey. Distinguishing Th1 and Th2 Cells. The Scientist, May 2001.
Gravenstein S, Duthie EH, Miller BA, Roecker E, Drinka P, Prathipati K, Ershler WB. Augmentation of influenza antibody response in elderly men by thymosin alpha one. A double-blind placebo-controlled clinical study. J Am Geriatr Soc. 1989 Jan;37(1):1-8.
Lim SG, Wai CT, Lee YM, Dan YY, Sutedja DS, Wee A, Suresh S, Wu YJ, Machin D, Lim CC, Fock KM, Koay E, Bowden S, Locarnini S, Ishaque SM. A randomized, placebo-controlled trial of thymosin-alpha1 and lymphoblastoid interferon for HBeAg-positive chronic hepatitis B. Antivir Ther. 2006;11(2):245-53.
Chen H, He MY, Li YM. Treatment of patients with severe sepsis using ulinastatin and thymosin alpha1: a prospective, randomized, controlled pilot study. Chin Med J (Engl). 2009 Apr 20;122(8):883-8.
Danielli R, Fonsatti E, Calabrò L, Di Giacomo AM, Maio M. Thymosin α1 in melanoma: from the clinical trial setting to the daily practice and beyond. Ann N Y Acad Sci. 2012 Oct;1270:8-12.
Schulof RS, Lloyd MJ, Cleary PA, Palaszynski SR, Mai DA, Cox JW Jr, Alabaster O, Goldstein AL. A randomized trial to evaluate the immunorestorative properties of synthetic thymosin-alpha 1 in patients with lung cancer. Journal of Biological Response Modifiers [01 Apr 1985, 4(2):147-158].
Luigina Romani, Francesco Bistoni, Roberta Gaziano, Silvia Bozza, Claudia Montagnoli, Katia Perruccio, Lucia Pitzurra, Silvia Bellocchio, Andrea Velardi, Guido Rasi, Paolo di Francesco and Enrico Garaci. Thymosin α 1 activates dendritic cells for antifungal Th1 resistance through Toll-like receptor signaling. Blood 2004 103:4232-4239.
stylecomfy. New drug (Thymosin alpha 1) discovery: potential for Cystic Fibrosis treatment. cysticfibrosis.com.
Matteucci C, Grelli S, Balestrieri E, Minutolo A, Argaw-Denboba A, Macchi B, Sinibaldi-Vallebona P, Perno CF, Mastino A, Garaci E. Thymosin alpha 1 and HIV-1: recent advances and future perspectives. Future Microbiol. 2017 Feb;12:141-155.
Thymosin Beta-4. ScienceDirect.
Chang CH, Tsai WC, Lin MS, Hsu YH, Pang JH. The promoting effect of pentadecapeptide BPC 157 on tendon healing involves tendon outgrowth, cell survival, and cell migration. J Appl Physiol (1985). 2011 Mar;110(3):774-80.
Hsieh MJ, Liu HT, Wang CN, Huang HY, Lin Y, Ko YS, Wang JS, Chang VH, Pang JS. Therapeutic potential of pro-angiogenic BPC157 is associated with VEGFR2 activation and up-regulation. J Mol Med (Berl). 2017 Mar;95(3):323-333.
Chang CH, Tsai WC, Hsu YH, Pang JH. Pentadecapeptide BPC 157 enhances the growth hormone receptor expression in tendon fibroblasts. Molecules. 2014 Nov 19;19(11):19066-77.
Plosker, G.L. & Gauthier, S. Cerebrolysin. Drugs Aging (2009) 26: 893.
Muresanu DF, Heiss WD, Hoemberg V, et al. Cerebrolysin and Recovery After Stroke (CARS): A Randomized, Placebo-Controlled, Double-Blind, Multicenter Trial. Stroke. 2016;47(1):151–159.
Ghaffarpasand F, Torabi S, Rasti A, et al. Effects of cerebrolysin on functional outcome of patients with traumatic brain injury: a systematic review and meta-analysis. Neuropsychiatr Dis Treat. 2018;15:127–135. Published 2018 Dec 27.
Menon PK, Muresanu DF, Sharma A, Mössler H, Sharma HS. Cerebrolysin, a mixture of neurotrophic factors induces marked neuroprotection in spinal cord injury following intoxication of engineered nanoparticles from metals. CNS Neurol Disord Drug Targets. 2012 Feb;11(1):40-9.
Gavrilova SI, Kolykhalov IV, Fedorova IaB, Selezneva ND, Kalyn IaB, Roshchina IF, Odinak MM, Emelin AIu, Kashin AV, Gustov AV, Antipenko EA, Korshunova IuA, Davydova TA, Messler G. Possibilities of preventive treatment of Alzheimer's disease: results of the 3-year open prospective comparative study on efficacy and safety of the course therapy with cerebrolysin and cavinton in elderly patients with the syndrome of mild cognitive impairment. Zh Nevrol Psikhiatr Im S S Korsakova. 2010;110(1):62-9.
Sotnikova NY, Gromova OA, Novicova EA. Dual effect of cerebrolysin in children with attention deficit syndrome with hyperactivity: neuroprotection and immunomodulation. Russ J Immunol. 2002 Dec;7(4):357-64.
Ciobanu A, Petcu C, Surdu A. Cerebrolysin augmentation in treatment-resistant depression at elderly. 10th World Congress of Biological Psychiatry, May 31, 2011.
Tuthill CW, King RS. Thymosin Apha 1–A Peptide Immune Modulator with a Broad Range of Clinical Applications. Clin Exp Pharmacol 2013, 3:4.
Can Therapeutic Peptides Revolutionize the Future of Precision Medicine? was originally published on Dr. Jill's website on June 19, 2019; used with permission.